If you’ve ever looked in the mirror and wondered, “Why are some of my pimples tiny and others deep and painful?”, you’re not alone. Acne isn’t just one skin condition — it’s a broad spectrum of lesions that differ in cause, appearance, and treatment.
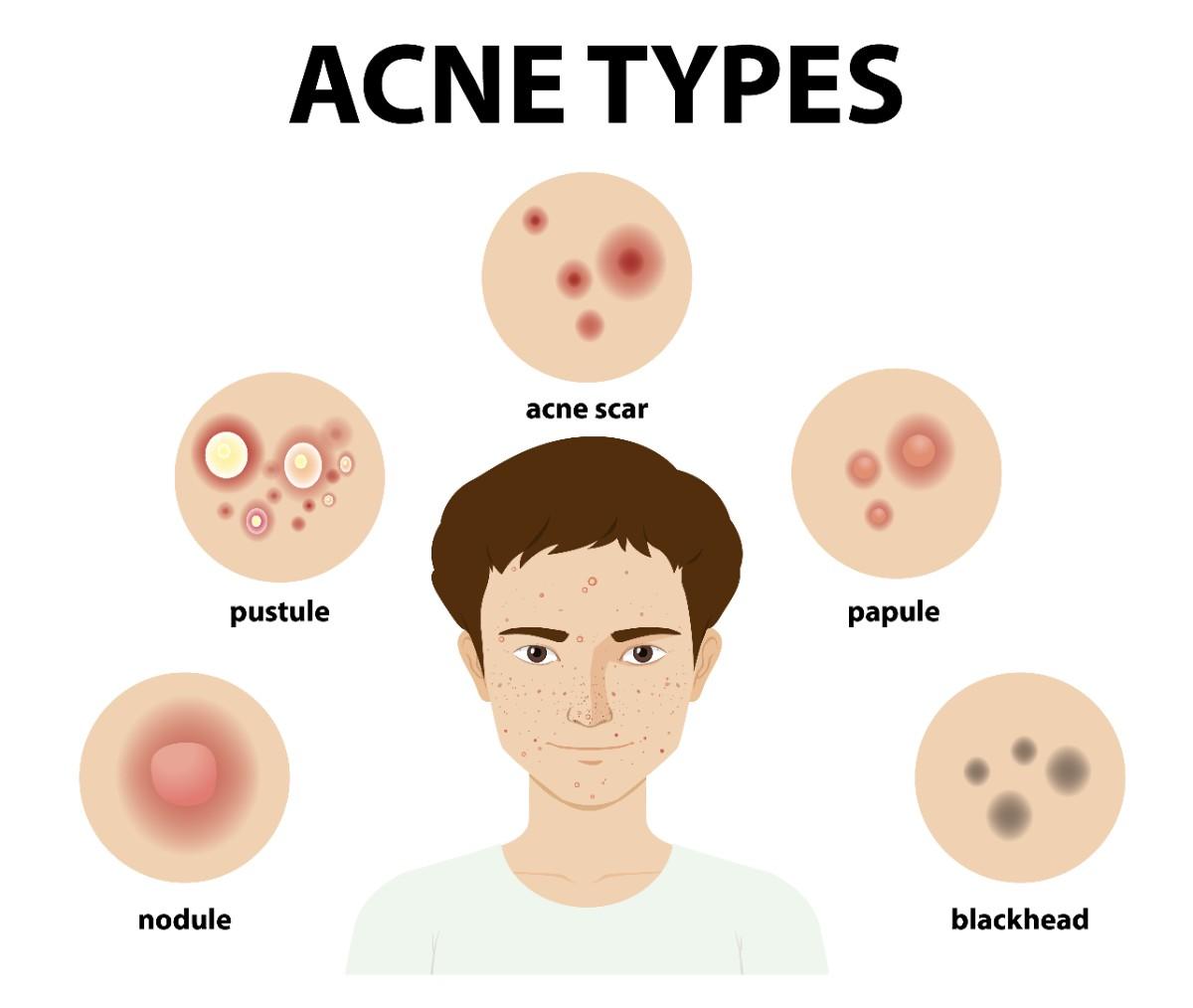
Dermatologists classify acne into several types, from non-inflammatory forms like blackheads and whiteheads to inflammatory types like papules, pustules, nodules, and cysts. Understanding these differences isn’t just about labels — it’s the key to choosing the right treatment and preventing long-term scarring.
In this detailed guide, we’ll break down the types of acne, their unique features, underlying causes, and how dermatologists treat each one effectively.
Understanding Acne Classification
Before we dive into individual types, it’s important to know how dermatologists categorize acne.
Broadly, acne is divided into two main groups:
-
Non-inflammatory acne (comedonal acne) — caused by clogged pores without redness or swelling.
-
Inflammatory acne — involves bacterial activity, redness, swelling, and deeper lesions.
While many people experience both forms simultaneously, recognizing which type dominates can help you and your dermatologist choose the most effective skincare plan.
Non-Inflammatory Acne Types
These are the milder forms of acne — often the starting point before inflammation develops. They result from clogged pores (comedones) due to oil, dead skin cells, and debris buildup.
1. Blackheads (Open Comedones)
What They Are:
What is acne? Blackheads are one of its common types — small, dark dots on the skin’s surface. Despite the myth, they aren’t dirt; their black color comes from oxidized sebum and dead cells exposed to air.
Where They Appear:
Most commonly on the nose, forehead, and chin (T-zone) — areas with high oil activity.
Causes:
-
Overproduction of sebum
-
Poor exfoliation or buildup of dead skin
-
Use of heavy or occlusive skincare products
Treatment:
-
Salicylic acid (BHA) helps unclog pores and reduce oil buildup.
-
Topical retinoids (Adapalene, Tretinoin) promote cell turnover and prevent blockage.
- Avoid pore strips — they may temporarily remove debris but irritate and enlarge pores over time.
“Consistency, not aggression, is the secret to clearer skin. Gentle exfoliation helps prevent clogged pores and blackheads without damaging the skin barrier.”
Dr. Whitney Bowe, MD, FAAD — Board-Certified Dermatologist & Clinical Assistant Professor, Mt. Sinai Hospital
2. Whiteheads (Closed Comedones)
What They Are:
Whiteheads form when a pore is clogged and closed at the surface, trapping sebum and bacteria beneath the skin. They look like small, white bumps — often mistaken for milia.
Where They Appear:
Cheeks, forehead, and jawline.
Causes:
-
Excess oil production
-
Hormonal fluctuations
-
Use of comedogenic (pore-clogging) makeup or skincare
Treatment:
-
Retinoids remain first-line therapy to normalize skin cell shedding.
-
Niacinamide reduces oil production and inflammation.
-
Maintain a non-comedogenic skincare routine — avoid heavy creams and silicone-based primers.
Pro Tip:
Never pop whiteheads. It increases the risk of post-inflammatory hyperpigmentation (PIH) and scarring.
Inflammatory Acne Types
These are more severe and often painful, caused by bacterial activity (Cutibacterium acnes) and the body’s inflammatory response. The lesions are red, swollen, and can lead to long-term marks.
3. Papules
Description:
Small, red, raised bumps without visible pus. Touching or squeezing them can worsen inflammation.
Causes:
-
Bacterial infection in clogged pores
-
Immune system reaction to trapped debris
Treatment:
-
Topical benzoyl peroxide to kill acne-causing bacteria
-
Gentle cleansers and fragrance-free moisturizers to calm skin
-
Avoid picking — it can convert papules into pustules or scars
4. Pustules
Description:
Pustules are similar to papules but contain visible white or yellow pus in the center. They often cluster on the face, chest, and back.
Treatment:
-
Benzoyl peroxide and salicylic acid for surface lesions
-
Topical antibiotics (clindamycin, erythromycin) under prescription
-
If widespread, dermatologists may prescribe short-term oral antibiotics
Note:
Spot treatments can help pustules heal faster, but they don’t prevent new ones — consistent full-face care is essential.
5. Nodules
Description:
Large, firm, painful bumps located deep under the skin’s surface. Unlike surface acne, nodules don’t come to a head and can last for weeks or months.
Causes:
-
Severe inflammation
-
Hormonal imbalance
-
Genetic predisposition
Treatment:
-
Oral retinoids (Isotretinoin) for resistant cases
-
Corticosteroid injections for rapid inflammation reduction
-
Oral antibiotics for moderate cases
Nodular acne almost always requires professional treatment — ignoring it can lead to permanent scarring.
6. Cysts
Description:
Cystic acne is the most severe form — large, pus-filled lesions deep beneath the skin, often painful to touch. They can merge into clusters and cause deep scars.
Causes:
-
Hormonal imbalances (common in adult women)
-
Genetic tendency to overproduce oil
-
Stress and poor skin barrier health
Treatment:
-
Isotretinoin (Accutane): The gold-standard prescription for cystic acne.
-
Corticosteroid injections to reduce swelling.
-
Laser and light therapies for long-term scar management.
“Once acne becomes cystic, over-the-counter products usually aren’t enough. You need a dermatologist to tailor a treatment plan — often involving oral medications or in-office therapies”
Dr. Mona Gohara, MD, FAAD — Associate Clinical Professor, Yale School of Medicine
Special Acne Variants
Beyond the common types, dermatologists also recognize specific variants triggered by friction, yeast, or hormonal fluctuations.
1. Acne Mechanica
-
Caused by heat, sweat, and friction (helmets, masks, tight clothing).
-
Common in athletes or people wearing PPE for long hours.
-
Prevention: Loose clothing, gentle cleansing after workouts, avoid prolonged friction.
2. Fungal Acne (Malassezia Folliculitis)
-
Technically not true acne — caused by yeast, not bacteria.
-
Appears as itchy, uniform bumps on chest, shoulders, and back.
-
Treatment: Antifungal cleansers or creams (ketoconazole, zinc pyrithione) — not benzoyl peroxide or retinoids.
3. Hormonal Acne
-
Fluctuates around menstrual cycles or PCOS.
-
Appears along jawline, chin, and lower face.
-
Treatment: Hormonal therapy (birth control pills, spironolactone), retinoids, and anti-inflammatory diets.
4. Acne Conglobata
-
Rare, severe acne with interconnected cysts and tunnels under the skin.
-
Can leave deep scars.
-
Requires isotretinoin or systemic steroids under dermatologic care.
5. Acne Fulminans
-
Extremely rare, sudden-onset, ulcerative acne with fever and joint pain.
-
A medical emergency requiring systemic treatment.
How to Identify Your Acne Type
You can often distinguish acne types by appearance and sensation:
| Feature | Non-inflammatory (Blackheads, Whiteheads) | Inflammatory (Papules, Pustules, Nodules, Cysts) |
| Color | White, black, or skin-colored | Red, swollen, or pus-filled |
| Pain | Usually painless | Often tender or painful |
| Depth | Surface-level | Deeper under skin |
| Treatment | OTC exfoliants, retinoids | Prescription medications, procedures |
If you’re unsure, it’s best to see a board-certified dermatologist for an accurate diagnosis. Misidentifying your acne type often leads to ineffective or aggravating treatments.
Dermatologist-Recommended Treatments by Type
| Acne Type | Common OTC Options | Prescription Options | In-Clinic Treatments |
| Blackheads / Whiteheads | Salicylic acid, retinoids | Adapalene, tretinoin | Chemical peels, comedone extraction |
| Papules / Pustules | Benzoyl peroxide | Antibiotics, retinoids | Blue light therapy |
| Nodules / Cysts | — | Isotretinoin, hormonal therapy | Cortisone injections, laser therapy |
| Fungal Acne | Antifungal wash | Oral antifungals | — |
| Hormonal Acne | — | Spironolactone, birth control pills | Laser or chemical peel adjuncts |
Pro Insight:
Acne treatment isn’t “one-size-fits-all.” A dermatologist tailors therapy based on type, severity, and your skin’s tolerance.
When to See a Dermatologist
If your acne:
-
Persists beyond 8–12 weeks of over-the-counter care
-
Causes pain, scarring, or dark marks
-
Triggers emotional distress or confidence issues
-
Appears suddenly and severely
It’s time to seek professional evaluation. Dermatologists can combine topical, oral, and procedural treatments to clear your skin safely and effectively.
FAQs
1. Are blackheads and whiteheads the same thing?
No. Blackheads are open pores exposed to air (oxidized), while whiteheads are closed and remain under the surface.
2. Can cystic acne go away on its own?
Unlikely. Cystic acne usually requires medical treatment to prevent scarring and recurrence.
3. How can I tell if my acne is hormonal?
If it flares around your period or along the jawline, it may be hormonal. Consult your dermatologist for evaluation.
4. Is it safe to pop pimples?
No. Popping spreads bacteria, delays healing, and increases scarring risk.
5. What’s the best acne treatment for sensitive skin?
Start with low-strength retinoids and gentle, non-comedogenic products. Introduce actives gradually under guidance.
Dermatologist’s Insight
“Each acne type tells a different story about your skin. Accurate identification and early treatment prevent years of frustration and scarring.”
— Dr. Alina Verma, MD (Dermatology)
Conclusion
Acne may take many forms — from small blackheads to deep cysts — but the underlying message is the same: every type is treatable with the right approach. Understanding your acne type empowers you to choose effective treatments, avoid triggers, and seek timely professional help.
Clear skin doesn’t happen overnight, but with consistency, care, and expert guidance, it’s absolutely achievable.
Medical Disclaimer
This article is for informational purposes only and not a substitute for professional medical advice. Always consult a board-certified dermatologist for diagnosis and personalized treatment.
Leave a Reply